Treatment options for pancreatic cancer
Pancreatic cancer is potentially curable in a small number of cases if it can be removed, but the vast majority of cases are not diagnosed until too late. Pancreatic cancer (adenocarcinoma) is one of the most devastating cancers with generally poor progress. There is however hope, in particular when surgery is possible.
On this page:
> Surgery
> Chemotherapy
> Radiation therapy
> Stent insertion and bypass surgery
> Being referred to a specialist centre
> Your treatment team
Surgery
When imaging suggests that the entire tumor can be removed and there is no evidence of obvious spread to other organs, surgical removal can be considered and may achieve cure. No other therapy can cure pancreatic cancer. Five-year survival rates approach 25% if the cancers are surgically removed while they are still small and have not spread to the lymph nodes.
Most curative surgery is designed to treat cancers in the head of the pancreas, near the bile duct. Some of these cancers are found early enough because they block the bile duct and cause jaundice. There is evidence that surgical complications are lower and survival is improved when pancreatic cancer surgery is performed at specialised centers, compared to surgery performed at hospitals where pancreatic cancer surgery is not commonly performed. (Pieper D et al. State of evidence on the relationship between high-volume hospitals and outcomes in surgery: a systematic review of systematic reviews. J Am Coll Surg 2013).
About 10-25% of pancreatic cancers are contained within the pancreas at the time of diagnosis allowing surgery to be considered. In many cases cancer cells too few to detect may already have spread to other parts of the body. This may explain why the cancer recurs in a large portion of patients after surgical removal.
Additional reading:
> Questions to ask your surgeon
> Questions to ask your oncologist
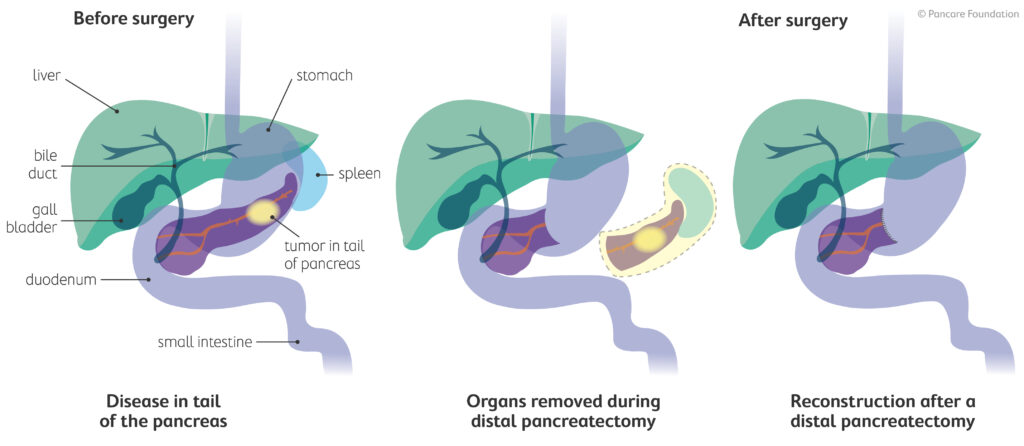
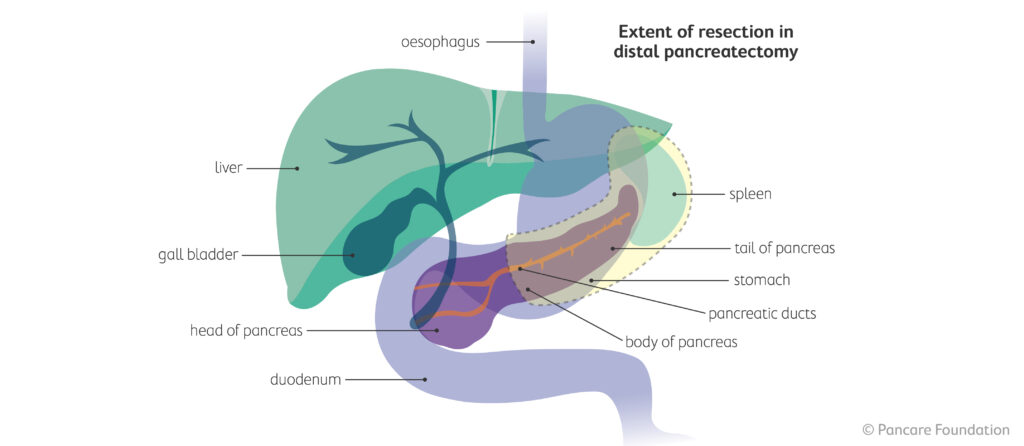
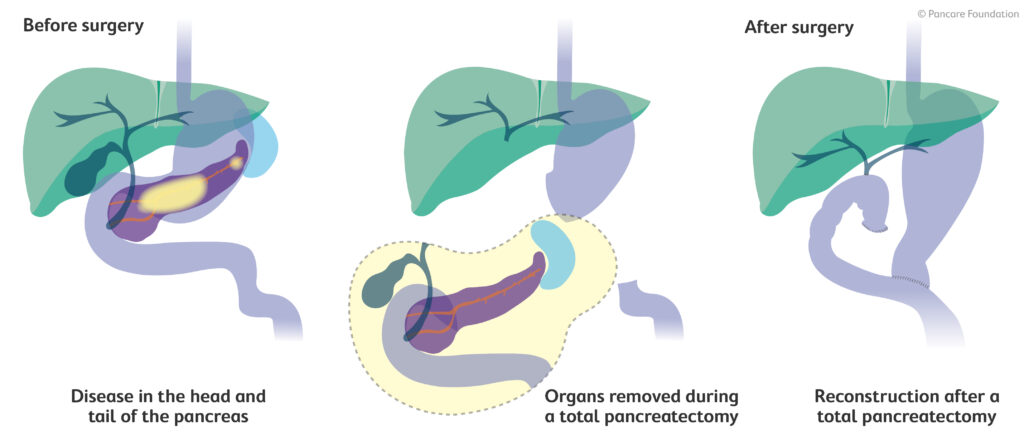
The type of surgery performed is guided by the location of the tumour. In cases of cancers within the head of the pancreas, a pancreaticoduodenectomy is most commonly performed. Also known as the Whipple’s procedure, this operation removes:
- Head of the pancreas
- Lymph nodes near the pancreas
- Gallbladder
- Part of the common bile duct
- Part of the stomach
- Duodenum (first part of the small intestine)
- A small portion of the jejunum (second part of the small intestine)
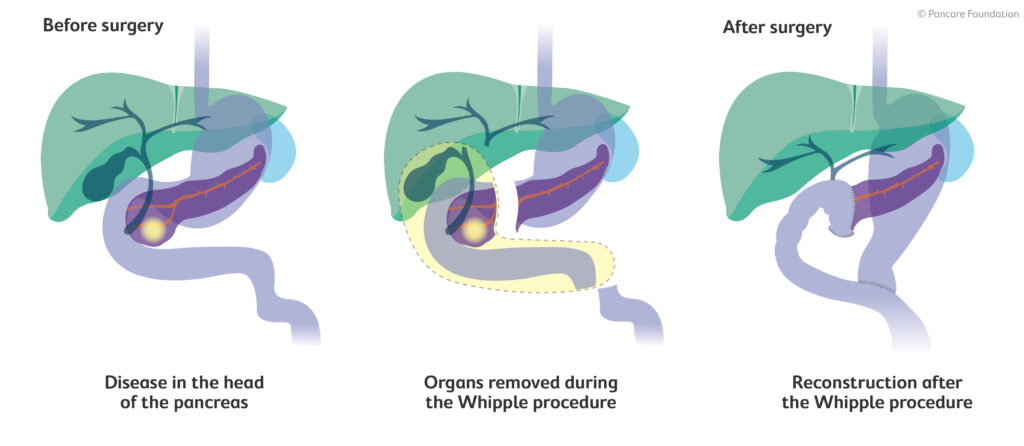
This is a complex operation and outcomes are generally optimal when the surgery is performed by a specialised surgeon who has performed many of these operations at a hospital with extensive experience in pancreatic surgery. Even in the most experienced centers, there is a 1-5% chance of death related to surgery within the first 30 days after surgery. Complications occur in 30-50% of patients. However, most complications do not cause major long-term debility and can be managed by relatively simple means.
Chemotherapy
Chemotherapy is offered to all patients with pancreatic cancer, even when tumor removal is achieved. This reduces the risk of the cancer returning. Chemotherapy is often used on its own to treat pancreas cancer that has spread and may lengthen survival. Given the generally poor prognosis of pancreatic adenocarcinoma, patients should strongly consider being involved in treatment trials if they are available. Always ask your oncologist if a clinical trial for treatment of pancreatic cancer is available in your region.
You may read or hear about various types of chemotherapy. Some common terms about chemotherapy include adjuvant and neoadjuvant. The term adjuvant in this setting refers to additional therapies added to the primary therapy, e.g. adjuvant chemotherapy was given after surgery. Neoadjuvant therapy simply means that the additional therapy is provided prior to the primary therapy, e.g. neoadjuvant chemotherapy was given before surgery.
Radiation therapy
Radiation therapy combined with low dose of chemotherapy may be used to reduce the chances of the cancer returning locally. Radiotherapy is rarely required for the treatment of pancreatic cancer. Sometimes radiotherapy is administered in cases of more advanced cases to try and reduce the tumor size, with the hope of allowing subsequent surgical removal. It may also be offered to treat certain symptoms or when there is residual cancer noted after surgical removal of the tumor.
Stent insertion and bypass surgery
Some surgical and other interventional procedures are used that don’t remove the cancer but instead help relieve symptoms.
The cancer may have grown so that it blocks your duodenum or your bile duct. If your duodenum is blocked, food can’t get through to your bowel and builds up in your stomach, causing discomfort, sickness and vomiting. If your bile duct is blocked you may develop jaundice, with symptoms such as yellowing of the skin and eyes and itching.
In both cases a small, flexible plastic or metal tube called a stent can be inserted to relieve a blockage and keep the duct or bowel open. Stents to unblock the bile duct are most often put in during an ERCP. If this isn’t possible an alternative procedure called a PTC (Percutaneous Transhepatic Cholangiogram) may be used. Here the stent is inserted directly through the skin and liver into the top of the bile duct using a needle and x-ray guidance.
Alternatively, surgeons can carry out an operation to bypass an actual or anticipated blockage. This is also performed at the time of surgery to remove the cancer, when cancer removal has proved not to be possible.
There are generally two components to a bypass operation that relates to pancreatic cancer and are as follows;
- when the stomach is blocked or at danger of blocking, the part of the small bowel just below the duodenum is connected directly to your stomach so that food can pass from the stomach into the bowel.
- For a blocked bile duct or a bile duct a danger of blocking, the duct is cut above the blockage and reconnected to the small bowel, allowing the bile to flow again.
Sometimes these two procedures are done at the same time.
Being referred to a specialist centre
Anyone diagnosed with pancreatic cancer should have their case reviewed at a centre where there is a specialist multidisciplinary team of doctors who are able to assess and treat the disease.
Guidelines from several countries suggest that surgery is preferably carried out in specialist centres that see and treat a ‘high volume’ of pancreatic cancer patients. The outcomes of pancreatic surgery in particular appears to be better in high volume centres who perform at least 10-20 pancreatic operations per year, by surgeons that are perform at least 5 pancreatic resections per year (Pecorelli N et al. Effect of surgeon volume on outcome following pancreaticoduodenectomy in a high -volume hospital. J Gastrointestinal surgery 2012).
Hospitals in a region often work together with the specialist centres to try to ensure the best treatment and care for all patients close to home. You may find it is not necessary for you to travel to a specialist centre for all investigations. Many tests and investigations can be done at your local hospital and standard chemotherapy can often be given there as well.
However, local hospitals may not always be involved in running clinical trials or offer all the treatments available at specialist centres. Therefore, if you are considering taking part in a particular clinical trial you may need to travel in order to have your treatment.
Treatment Team
Depending on your treatment, your treatment team may consist of a number of different health professionals, such as:
- General Practitioner – your GP looks after your general health and works with your specialists to coordinate treatment
- Gastroenterologist – specialises in diseases of the digestive system, can also perform endoscopy procedures
- Upper gastrointestinal (UGI) surgeon – specialises in surgery to treat diseases of the upper gastrointestinal system
- Medical oncologist – prescribes and coordinates chemotherapy treatment
- Radiation oncologist – prescribes and coordinates radiation therapy treatment
- Cancer nurses – assist with treatment and provide information and support throughout your treatment
- Other allied health professionals – such as dietitians, exercise physiologists, social workers, pharmacists, speech pathologists and counsellors.
Read more:
> Side effects you may experience from treatment